Hematopoietic stem cell transplantation (HSCT) is the only curative therapy for primary hemophagocytic lymphohistiocytosis (HLH). Conventional myeloablative conditioning regimen using busulfan, cyclophosphamide with or without etoposide was associated with high rate of transplant-related mortality (Horne et al. BJH 2005). Reduced intensity conditioning (RIC) is used in HLH to minimize transplant-related toxicities. The use of alemtuzumab, fludarabine, and melphalan in HLH was associated with low mortality; however, mixed donor chimerism and graft failure were frequent (Allen et al. Blood 2018). A recent report in 25 HLH patients who underwent HSCT from HLA matched donors using targeted busulfan (45-65 mg/L X h), fludarabine, and serotherapy resulted in adequate stable donor chimerism, no graft rejection, and no mortality (Felber et al. Blood Adv. 2020). In this study, we reviewed the outcome of 16 HLH patients who underwent HSCT from HLA matched donors using RIC.
All patients were initially treated using HLH-2004 protocol. They subsequently underwent HSCT from 10/10 HLA matched related or unrelated donor using RIC regimens. We initially used AFM conditioning regimen that included alemtuzumab (1 mg/kg), fludarabine (150 mg/m2), and melphalan (140 mg/m2) with or without thiotepa (10 mg/kg). GVHD prophylaxis included cyclosporine (CSA) and steroids. Given the high rate of low donor chimerism with AFM regimen, we subsequently used BF conditioning regimen that included busulfan (weight-based dosing for total of 16 doses) and fludarabine (160 mg/m2). Therapeutic drug monitoring of busulfan was performed. Thymoglobulin (10 mg/kg) was added in matched unrelated donor (MUD). GVHD prophylaxis included CSA and steroids in matched related donors (MRD) and CSA and methotrexate in MUD. Bone marrow was the stem cell source in all patients except one who underwent second transplant using peripheral blood stem cells. Supportive care was consistent among all patients. Defibrotide prophylaxis was administered to prevent sinusoidal obstruction syndrome (SOS). Donor chimerism <5% from whole blood or <20% in T-cell, graft failure, and death from any cause were considered as events.
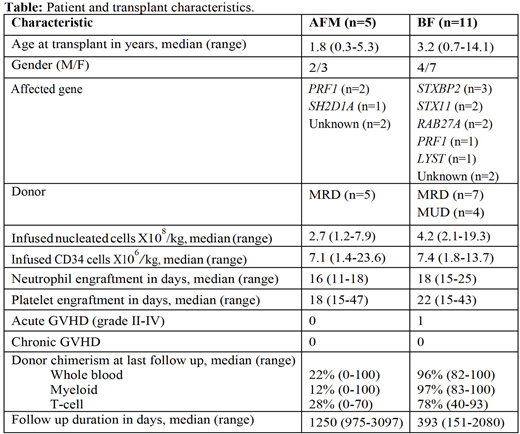
A total of 16 HSCT transplants were performed, 5 received AFM regimen and 11 received BF regimen. Patient and transplant characteristics are shown in Table. All patients had successful neutrophil and platelet engraftments. Among the five patients who underwent AFM conditioning, one patient with SH2D1A mutation is 8 years post transplant with stable full donor chimerism and another patient with PRF1 mutation who received AFM with thiotepa has stable sufficient donor chimerism 3 years post transplant. Both patients did not require donor leukocyte infusions (DLI). The remaining 3 patients had declining donor chimerism beyond the first year of transplant despite the frequent use of DLI, one of them had disease reactivation and underwent second HSCT using BF regimen. Event free survival (EFS) at 3 years
was 60% and overall survival (OS) was 100%. Among the 11 patients who underwent BF regimen, 7 were transplanted using MRD and 4 MUD. The median cumulative area under the curve of busulfan was 64 mg/L X h (range, 56-73). Median donor myeloid chimerism was 97% (range, 83-100) and median T-cell chimerism was 78% (range, 40-93). One patient who underwent MUD had grade III acute GVHD and none had chronic GVHD. Two patients had mild SOS. There were no events among BF group with median follow up duration of 393 days (151-2080).
The use of BF regimen in HLH was associated with excellent outcome and stable donor chimerism with no graft failure in comparison to AFM regimen. Longer follow up is needed to confirm our findings.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal